How to Reduce Overdue Dental Insurance Claims
Your aging report keeps growing, and the list of insurance claims past thirty days is starting to look like a to-do list no one ever gets to. Follow-up happens only when someone has a quiet moment, which hardly ever comes. If you feel like the overdue claims pile is quietly eating into your collections, you’re not alone.
What this problem actually looks like
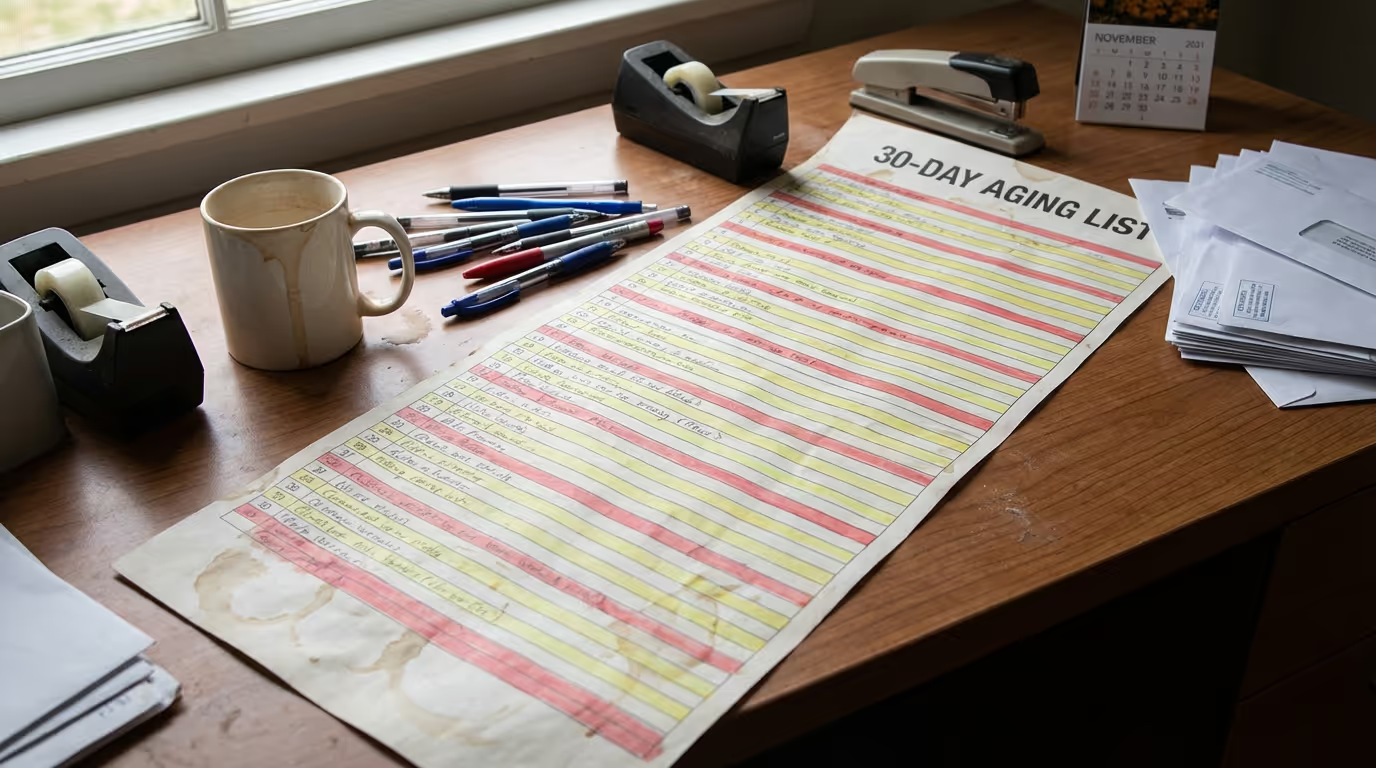
I’ve worked the front lines of dental billing, and I remember the days when we’d walk into the morning huddle with twenty claims already past due, knowing another ten would hit the thirty-day mark by week’s end. Sometimes it was a new insurance rep needing the same x-rays we’d sent twice. Other times, it was simply no one having had the bandwidth to check on the claims queue since Monday. Most teams want to stay on top of aging claims, but it’s easy for this stuff to get buried under today’s patients, last-minute schedule changes, and a stack of EOBs still needing to be posted.
In one office I managed, our system was to print the full outstanding claim list every Friday before lunch. You’d think printing it would force us to handle it—we got as far as highlighting the worst offenders. But Monday would arrive, and the dog-eared list was shoved under the mouse pad by noon. It’s usually not laziness, just too many things on too few plates. The peace of mind that comes with a clean AR report starts to feel out of reach, especially when everyone is just trying to keep the lights on and the next patient moving.
Where this usually breaks and what it costs
The cracks show in small, daily ways. Claims are sent without checking if the frequency or missing tooth clause applies. You submit before a picture gets scanned or before verifying if the patient maxed out their benefits last month. A claim sits pending because the insurance portal needed one more X-ray, but no one was told, and a simple “insufficient documentation” note gets buried in a portal no one checked. These are the small process misses that, over time, snowball into big financial headaches.
Even with the best of intentions, most offices just don’t have enough time to chase every claim, let alone root out process errors. Administrative work in dentistry is a massive lift, costing 3.2 billion dollars annually, with 2 billion that could be saved if routine transactions were handled more efficiently (CAQH Dental). In practice, this means insurance money sits in limbo while the clock keeps ticking on AR—and you end up spending more time and money fixing mistakes from claims gone stale. Give this a few “busy months,” and you’re easily looking at thousands in old, hard-to-collect insurance balances, frustrated staff, and a cash flow crunch that could have been avoided.
What we would do this week
- Pick a daily, nonnegotiable window—just 30 minutes—dedicated to insurance aging follow-up, with one lead person each day (rotate if possible).
- Update your claim submission checklist in Open Dental to include key pitfalls: frequency limits, missing tooth clause triggers, X-ray/image attachments, and prior eligibility checks.
- Run your oldest unpaid claim list by payer and claim type. Flag claims over 45 days. For these, assign and document next steps (call, portal message, or resubmit with attachments) directly in the Open Dental claim notes.
Where DayDream helps
DayDream blends experienced dental billers with automation and AI so overdue insurance claims are tracked proactively—not just when someone finds time. They handle the whole workflow, from insurance verification and claims submission to attachments, denials, and follow-up, all mapped straight from your PMS, portals, and bank systems. Their platform shows real-time dashboards for denials, claim status, and A/R trends, so office managers always know where money is stuck. Practices using DayDream cut about 60% of manual billing work and collect payments close to 50% faster—often saving 10–14 hours of admin time a week. DayDream’s automation handles the repetitive follow-up, while their people jump in wherever insurance quirks or judgment calls are needed.
If your overdue claims list has become a source of stress and missed revenue, you’re not alone. The reality is, no one means to let claims slip—it’s just the nature of dental admin today. There’s a smarter, more sustainable way. Take a breath, regroup, and if you need a true process lift, book a short consult.