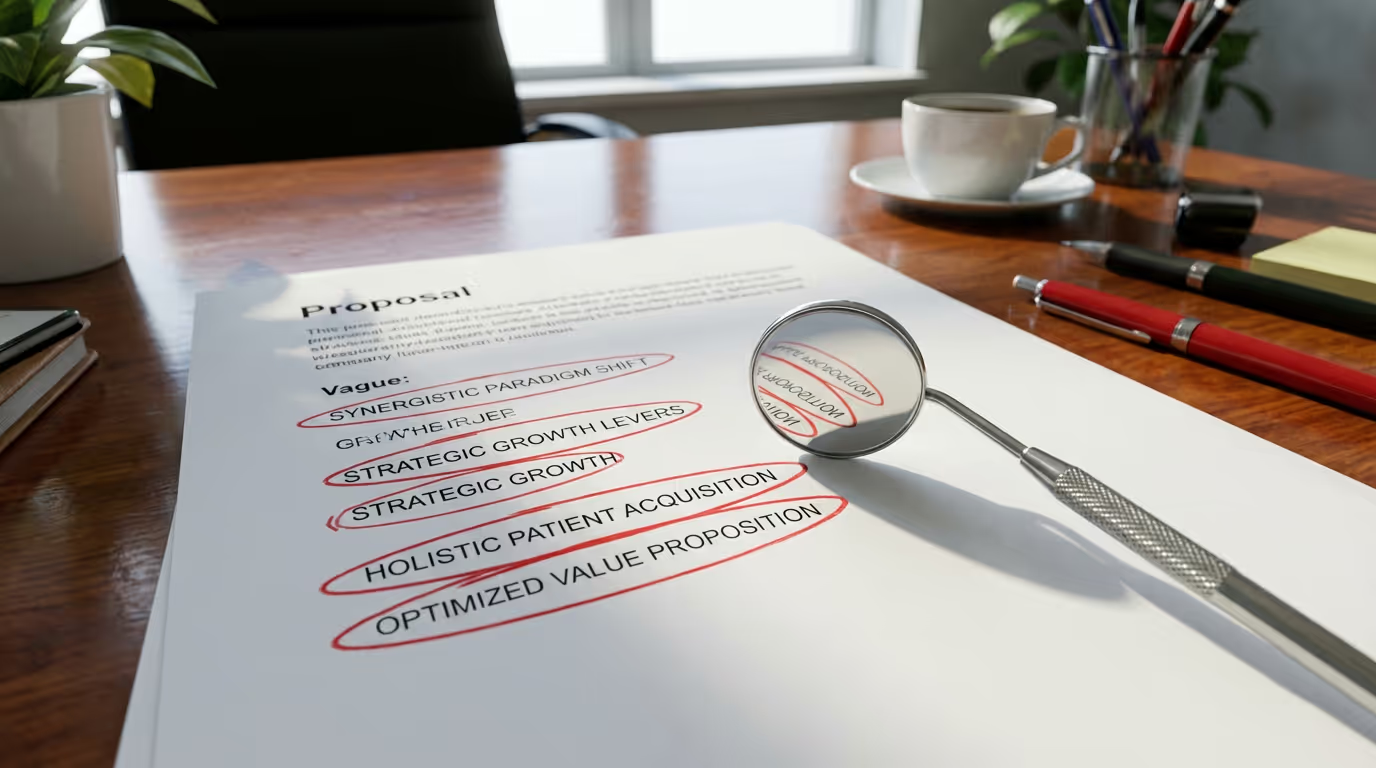
Top Red Flags in Outsourced Dental Billing Companies
I was once in your seat, reviewing proposals from billing companies that promised the moon yet left me uneasy. The language is always smooth—"raise your collections," "lighten admin load"—but under the surface, the details are thin. When you live at the front desk, you learn quickly that vague claims often hide more problems than they solve. Let’s talk honestly about recognizing red flags in a dental billing company, especially for Open Dental practices.
What this problem actually looks like
Here’s how it creeps in: You sign the contract, you meet your new billing “partner,” and the first weeks seem quiet. Then you notice unexplained adjustments appearing in your Open Dental ledger. Claims are being submitted, but the notes in the history read like canned copy-paste jobs. When I was tasked with clean-up, I’d find claim denials with no appeals filed, misspelled procedure codes, or worse—insurance verifications left on sticky notes, not in PMS fields. Once, I called a billing company about a payment that had disappeared on a Friday afternoon; their operator had no idea who posted it or how to trace it. Suddenly, “full visibility” meant logging into three portals just to double-check their work.
When billing companies cut corners on tasks like eligibility or batch up claims to run on a set schedule, you see the domino effect. Last-minute eligibility checks—if they bother at all—lead to patients showing up for hygiene only to find out their coverage maxed out last week. Sometimes payments get posted to the wrong provider, or write-offs get dumped under “miscellaneous.” These aren’t headline-grabbing failures, but they eat away at trust and force your team to triple-check what should have been simple. It’s not about catching one big error. It’s about a stream of micro-mistakes that drag your day down.
Where this usually breaks and what it costs
The most common breakdowns start with poor documentation and lack of transparency. If a billing company can’t explain its processes in plain language or show you exactly how they track claim status within Open Dental, you’re already on shaky ground. I’ve seen outsourced teams perform eligibility checks hours before an appointment—missing crucial downgrades or waiting period clauses—which leads to uncomfortable front-desk conversations and frustrated patients. That kind of sloppiness isn’t just inconvenient: eligibility errors are a significant driver of improper payments, which made up $51.6 billion across federal programs last year (CMS).
Every weak handoff—missing claim notes, unexplained adjustments, untracked appeals—multiplies the time staff spend untangling history, chasing status, or fighting denials. You might think you’re saving with an outside vendor, but when your A/R ratio creeps up or insurance write-offs climb, you start to pay for it elsewhere. About half of office managers report frequent problems with plan service, especially verification and claims (NADP/AADOM). Every time billing shortcuts force you to double-check their work, you lose time you’ll never get back—and staff trust wears thin.
What we would do this week
- Request a complete workflow map from your billing vendor, including who does what at each step, and insist they document how claim statuses are mapped and tracked in your Open Dental fields.
- Review a random week’s worth of posted payments and EOBs for accuracy, looking for unexplained write-offs, posting errors, or missing explanations in the claim notes.
- Hold a short team huddle to gather your front desk’s real observations: ask about the oddest or most frequent billing headaches since outsourcing (missed verifications, unclear adjustments, silences when things get denied) and note every single example.
Where DayDream helps
DayDream blends experienced dental billers with automation and AI, which means you don’t wonder if a real human is paying attention to your nuanced claims. Their team uses task-based workflows that integrate directly with your practice management software, so every piece of claim activity, insurance verification, and payment posting is visible to you in real time. Full benefit breakdowns show up about seven days ahead of appointments, mapped right into structured PMS fields, documenting frequencies, downgrades, waiting periods, and all the things that get lost in translation. Their technology automates repetitive tasks, allowing billers to operate two to three times more efficiently, and your payments arrive about fifty percent faster—all with dashboards showing up-to-the-minute status, denials, and trends.
Spotting the red flags in a dental billing company isn’t just about catching big promises; it’s about protecting your day-to-day sanity and your financial health. If you’re tired of living with hidden mistakes, unclear workflows, or silence when you need answers, you’re not alone. Let’s make it easier—book a short consult and see how you can get your billing working for you again.