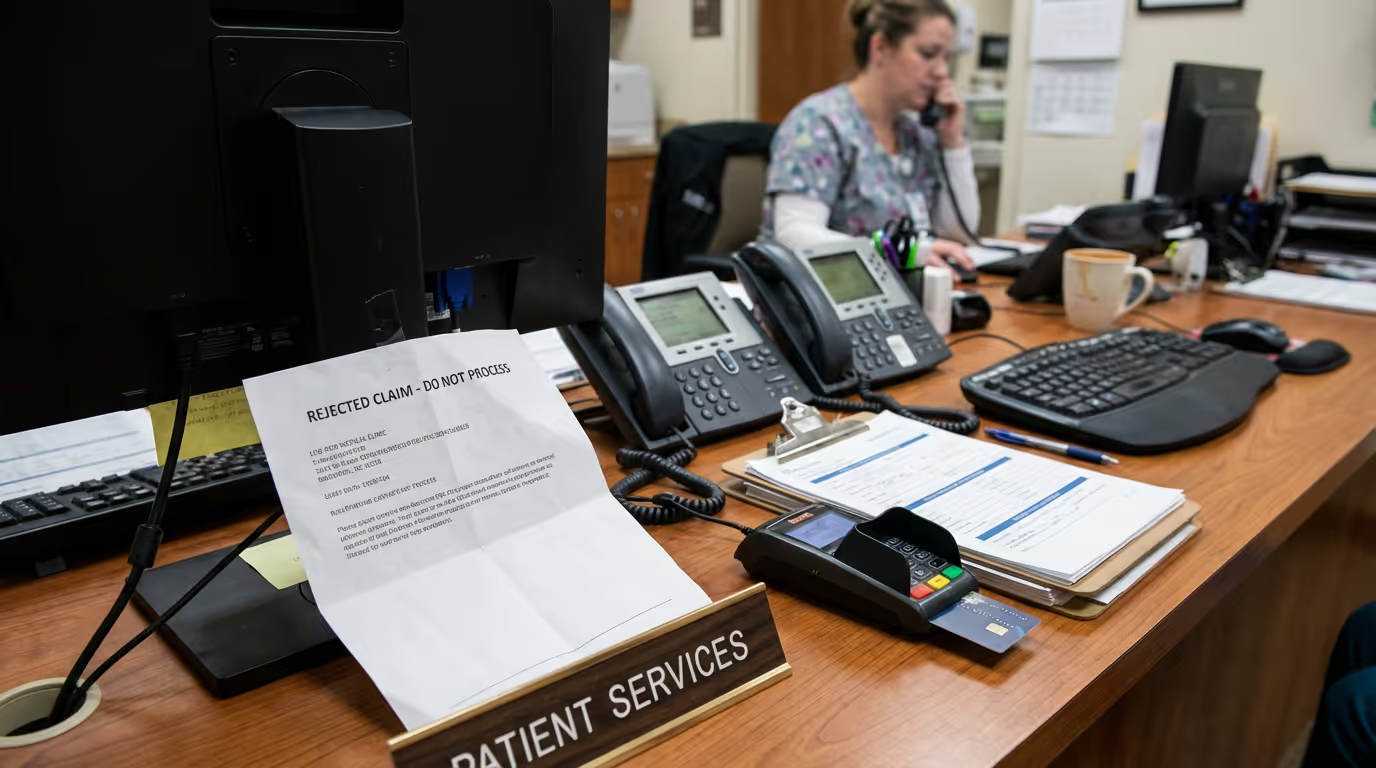
Should the Front Desk Handle Dental Billing?
Phones are ringing, someone is waiting to check in, and there’s a new patient halfway through a medical history when a denied claim pops up. I’ve lived it more times than I can count—a stack of EOBs stashed to the side, insurance calls on hold, and billing questions squeezed into the seconds between checking eligibility and greeting a child with a lost retainer. It’s normal for the front desk, but normal doesn’t mean it works well. The real-world problem here is simple: the front desk is forced to juggle vital dental office billing responsibilities with patient-facing tasks, and things slip in the rush.
What this problem actually looks like
In practical terms, here's what happens. You’re mid-sentence explaining the next recall visit when someone asks about an old balance from months ago. You promise to look into it, but then you need to check benefits for someone else now sitting in the operatory. That promise gets buried with good intentions, and AR ticks up quietly in the background. Or maybe, while registering a family of four, you get a payer portal timeout. You mean to resubmit yesterday’s denied claim, but it ends up on tomorrow’s pile. These moments add up. I’ve seen patient trust chipped away, and daily billing work pushed out by constant interruptions.
The worst is the domino effect. One missed eligibility check rolls into an estimate that’s off, an insurance downgrade missed, or an uncovered service gone unnoticed. You spend unpaid time calling patients and dealing with collections later. Patients lose confidence. The dental team is left frustrated, or even angry, arguing over why another claim bounced back or a write-off crept in. It never just costs time—there’s always a cost to trust, to cash flow, and to the team’s energy.
Where this usually breaks and what it costs
Conflicts and errors start where most people don’t see them: scattered workflows and split priorities. A front desk operator might switch between five systems within an hour—answering new patient calls, updating treatment plans, submitting new claims, checking eligibility for unforeseen procedures, handling walk-in questions, and updating the doctor about same-day insurance issues. Each handoff, each moment of divided attention, is a spot where dental office billing responsibilities at the front desk break down. The dental field is especially vulnerable since manual dental eligibility checks cost several times more than electronic ones. When eligibility checks or billing steps go unfinished, it’s not just claims that get delayed; verification spending alone jumped about fifteen percent in a single year to roughly two billion dollars, as offices struggle to piece coverage details together under time stress (EPDDS).
I’ve watched small things snowball. One incomplete claim submission ends up with weeks of back-and-forth with the insurer, extra patient calls, and then cash flow issues that affect paying staff. Some days it’s a miskeyed code; other times it’s missing a waiting period note or frequency limit in Open Dental. So much of this is shaped by how tight things get at the front. Even minor gaps mean more unpaid AR, more follow-up, and more stress—the stuff that makes billers or front desk staff want to pack it in. Sixty minutes lost every day adds up to thousands over the months and can quietly wear down even seasoned operators.
What we would do this week
- Map out every billing step your front desk handles—from eligibility checks in Open Dental to EFT posting—and highlight where patient check-in overlaps with insurance work.
- Batch eligibility verification and claim submission during low-traffic hours, and have a clear signpost for “urgent billing only” requests during rushes.
- Set auto-reminders in your PMS (like Open Dental) for tight AR follow-up and document every denied claim’s next action, even if it means a sticky note for now, so nothing falls through during front desk chaos.
Where DayDream helps
DayDream brings structure and relief by handling complex dental billing tasks so the front desk team can focus on patients. With full benefit breakdowns days ahead of every appointment, the right frequencies, downgrades, and tricky plan rules are mapped directly into Open Dental or your PMS fields by DayDream’s operators. Repetitive payment posting, insurance follow-up, and claim appeals are handled with a blend of dedicated billers and automation. With DayDream, the dental office lifts collections by about five percent and can save ten to fourteen admin hours a week by removing much of the manual work, leading to faster payments and real-time transparency.
I know how hard a front desk works, and how easy it is to get blamed for problems that start with an impossible workload. If billing is pulling you away from patients and keeps leaking out into after hours, you’re not alone. The core problem is never your hustle—it’s the broken system that asks you to do too much at once. For ideas, a better workflow, or to see what support could lighten your load, book a short consult.